Anúncios
A Type 2 diabetes diagnosis can feel overwhelming, but with resilience, knowledge, and proper management strategies, individuals can transform this challenge into an empowering journey toward better health.
Understanding the Initial Impact of a Type 2 Diabetes Diagnosis 🏥
The moment a healthcare provider delivers a Type 2 diabetes diagnosis marks a pivotal turning point in anyone’s life. The initial reaction often involves a complex mixture of emotions: shock, fear, denial, and sometimes relief at finally having an explanation for persistent symptoms.
Anúncios
Research indicates that approximately 37 million Americans live with diabetes, with 90-95% of these cases being Type 2 diabetes, according to the Centers for Disease Control and Prevention.
Understanding the psychological impact of this diagnosis is crucial for beginning the empowerment journey. Many individuals experience what healthcare professionals call “diabetes distress”—a unique emotional burden that differs from clinical depression but can significantly affect quality of life and disease management.
Anúncios
The diagnosis forces individuals to confront their mortality and lifestyle choices while simultaneously demanding immediate action. However, this critical juncture also presents an opportunity for positive transformation.
Unlike many chronic conditions, Type 2 diabetes responds remarkably well to lifestyle interventions, making it one of the most manageable chronic diseases when approached with determination and proper guidance.
The Science Behind Type 2 Diabetes: Knowledge as Power 📚
Empowerment begins with understanding the fundamental mechanisms of Type 2 diabetes. This condition occurs when the body becomes resistant to insulin or when the pancreas cannot produce sufficient insulin to maintain normal glucose levels. Insulin acts as a key that unlocks cells, allowing glucose from food to enter and provide energy.
When insulin resistance develops, glucose accumulates in the bloodstream rather than nourishing cells. Over time, elevated blood sugar levels can damage blood vessels, nerves, and vital organs. This explains why diabetes management focuses heavily on maintaining blood glucose within target ranges.
Several risk factors contribute to Type 2 diabetes development:
- Excess body weight, particularly abdominal fat
- Physical inactivity and sedentary lifestyle patterns
- Family history and genetic predisposition
- Age, with risk increasing after 45 years
- Ethnic background, with higher prevalence in certain populations
- Previous gestational diabetes or prediabetes diagnosis
- Polycystic ovary syndrome (PCOS)
- High blood pressure and abnormal cholesterol levels
Understanding these factors helps individuals identify which elements they can modify and which require medical management. This knowledge transforms patients from passive recipients of care into active participants in their health journey.
Building Your Diabetes Management Foundation 💪
Effective diabetes management rests on several interconnected pillars. The first involves assembling a comprehensive healthcare team. Beyond the primary care physician, this team might include an endocrinologist specializing in diabetes, a certified diabetes educator, a registered dietitian, an exercise physiologist, and mental health professionals when needed.
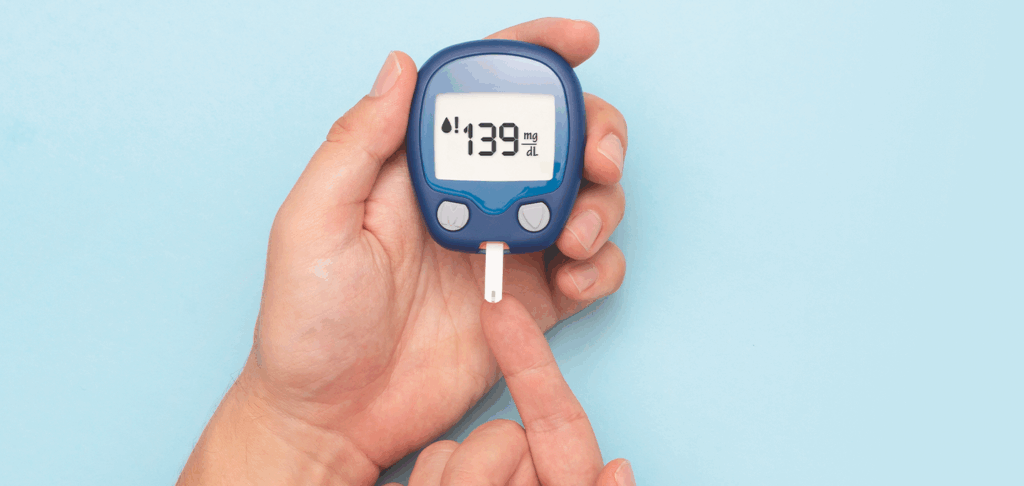
Regular monitoring forms another critical foundation element. Blood glucose testing provides immediate feedback about how food, activity, stress, and medication affect sugar levels. Many individuals benefit from continuous glucose monitors (CGMs) that provide real-time data without frequent finger pricks. These devices have revolutionized diabetes management by revealing patterns that traditional testing methods might miss.
Understanding target ranges is essential. The American Diabetes Association recommends fasting blood glucose between 80-130 mg/dL and postprandial (after-meal) levels below 180 mg/dL. However, targets should be individualized based on age, diabetes duration, comorbidities, and hypoglycemia risk.
The hemoglobin A1C test, performed every three to six months, provides an average blood glucose level over the previous two to three months. Most adults with diabetes should aim for an A1C below 7%, though individual targets may vary.
Nutrition: The Cornerstone of Diabetes Control 🥗
Dietary modifications represent one of the most powerful tools for managing Type 2 diabetes. Rather than viewing nutrition changes as restrictive, successful individuals reframe this aspect as an opportunity to discover nourishing, satisfying foods that support their health goals.
The plate method offers a simple, effective approach to meal planning. Visualize dividing a nine-inch plate: half should contain non-starchy vegetables, one quarter lean protein, and one quarter carbohydrates, preferably whole grains or starchy vegetables. This method naturally controls portions while ensuring balanced nutrition.
Carbohydrate counting and understanding glycemic index values help predict how foods affect blood sugar. Low glycemic index foods cause slower, smaller increases in blood glucose compared to high glycemic options. Pairing carbohydrates with protein, healthy fats, or fiber slows digestion and moderates blood sugar spikes.
Fiber deserves special attention in diabetes nutrition. Soluble fiber, found in oats, beans, apples, and citrus fruits, slows glucose absorption. Most adults should consume 25-35 grams of fiber daily, yet average intake falls significantly short. Gradually increasing fiber intake while staying adequately hydrated can improve glycemic control and support weight management.
Meal timing also matters. Regular eating schedules help maintain stable blood sugar levels and prevent extreme fluctuations. Some research suggests that front-loading calories earlier in the day may offer metabolic advantages, though individual responses vary.
Physical Activity: Moving Toward Better Health 🏃
Exercise represents another powerful intervention for Type 2 diabetes management. Physical activity increases insulin sensitivity, meaning cells can use available insulin more effectively. This effect persists for hours after exercise concludes, and regular activity produces lasting improvements in glycemic control.
The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity weekly, spread across at least three days, with no more than two consecutive days without exercise. Additionally, resistance training targeting all major muscle groups should occur at least twice weekly.
Aerobic activities include brisk walking, swimming, cycling, dancing, and gardening. The key is finding activities enjoyable enough to sustain long-term. Moderate intensity means exercising hard enough to raise heart rate and break a sweat while still being able to carry on a conversation.
Resistance training builds muscle mass, which increases metabolic rate and improves glucose utilization. Bodyweight exercises, resistance bands, free weights, or machine-based training all provide benefits. Working with a qualified fitness professional initially can ensure proper form and appropriate progression.
Breaking up sedentary time matters as much as structured exercise. Research shows that interrupting prolonged sitting with brief activity breaks every 30 minutes improves blood sugar control. Simple strategies include standing desk usage, walking meetings, parking farther away, or taking stairs instead of elevators.
Medication Management and Treatment Options 💊
While lifestyle modifications form the foundation of Type 2 diabetes management, many individuals also require pharmaceutical interventions. Metformin typically serves as the first-line medication due to its efficacy, safety profile, affordability, and potential cardiovascular benefits.
When metformin alone proves insufficient, numerous medication classes offer additional options. SGLT2 inhibitors help kidneys remove excess glucose through urine while providing cardiovascular and renal protection. GLP-1 receptor agonists enhance insulin secretion, slow gastric emptying, and often promote weight loss. DPP-4 inhibitors work similarly but with less pronounced effects.
Insulin therapy, once considered a last resort, is now recognized as an appropriate option at any disease stage when needed to achieve glycemic targets. Modern insulin formulations and delivery systems make therapy more convenient and precise than ever before.
Medication adherence significantly impacts outcomes. Strategies to improve adherence include using pill organizers, setting smartphone reminders, linking medication timing to daily routines, and understanding how each medication works. Open communication with healthcare providers about side effects, costs, or concerns enables timely adjustments.
Technology Tools Supporting Diabetes Management 📱
Digital health tools have transformed diabetes management, making tracking and analysis more accessible. Smartphone applications help users log blood glucose readings, meals, physical activity, medications, and symptoms while identifying patterns and trends.
Many apps integrate with glucose meters and continuous glucose monitors, automatically uploading readings and generating reports for healthcare providers. Some offer food databases with carbohydrate counts, barcode scanning features, and personalized insights based on individual responses to different foods.
Telehealth platforms enable remote consultations with diabetes educators, dietitians, and physicians, increasing access to specialized care regardless of geographic location. Virtual support groups connect individuals facing similar challenges, reducing isolation and fostering community.
Wearable fitness trackers monitor physical activity, sleep patterns, and heart rate, providing comprehensive data about factors affecting diabetes management. Integration between different devices and applications creates a holistic picture of health status and progress.
Emotional Resilience and Mental Health Considerations 🧠
The psychological aspects of living with Type 2 diabetes require as much attention as physical management. Diabetes distress, characterized by worry, frustration, and burnout related to disease management, affects a significant percentage of individuals with diabetes.
Recognizing signs of diabetes distress—feeling overwhelmed by management demands, worrying excessively about complications, experiencing guilt after blood sugar elevations, or feeling alone in the diabetes journey—enables early intervention. Healthcare providers can screen for diabetes distress using validated questionnaires and connect individuals with appropriate resources.
Cognitive behavioral therapy and mindfulness-based interventions show promise for reducing diabetes distress and improving self-management behaviors. These approaches help individuals identify unhelpful thought patterns, develop coping strategies, and cultivate self-compassion.
Building resilience involves developing realistic expectations, celebrating small victories, learning from setbacks without harsh self-judgment, and maintaining perspective. Diabetes management is a marathon, not a sprint, and perfectionism often undermines long-term success.
Social support plays a crucial role in psychological wellbeing. Sharing experiences with family members, friends, or diabetes support groups reduces isolation and provides practical assistance. However, setting boundaries around diabetes-related conversations and pushing back against unhelpful comments or unsolicited advice maintains healthy relationships.
Preventing Complications Through Proactive Care 🛡️
While focusing on daily management, individuals must also prioritize preventive care to minimize complication risks. Comprehensive diabetes care includes regular screenings and monitoring beyond blood glucose levels.
Annual eye examinations detect diabetic retinopathy before vision loss occurs. Early detection and treatment can prevent or delay progression. Similarly, regular kidney function tests through blood work and urine analysis identify diabetic nephropathy in treatable stages.
Foot care deserves special attention since diabetes increases risks of neuropathy, poor circulation, and slow wound healing. Daily foot inspections, proper footwear, prompt attention to minor injuries, and regular podiatric evaluations prevent serious complications requiring hospitalization or amputation.
Cardiovascular disease represents the leading cause of mortality in people with diabetes. Blood pressure and cholesterol management, often requiring medication alongside lifestyle modifications, significantly reduces cardiovascular risk. Many individuals with diabetes benefit from statin therapy regardless of baseline cholesterol levels.
Dental health connects to diabetes control in bidirectional ways. Periodontal disease makes blood sugar control more difficult, while elevated glucose levels increase infection risks. Regular dental cleanings and examinations, proper oral hygiene, and prompt treatment of gum problems support overall diabetes management.
Creating Sustainable Lifestyle Changes 🌱
Transforming a diabetes diagnosis into an empowering journey requires sustainable lifestyle changes rather than temporary fixes. Behavior change science offers insights into creating lasting habits.
Starting small increases success likelihood. Rather than overhauling every aspect of life simultaneously, focusing on one or two changes allows new behaviors to become established before adding more. This approach prevents overwhelm and builds confidence through successive achievements.
Implementation intentions, or “if-then” plans, strengthen habit formation. For example: “If it’s 7 AM on a weekday, then I will walk for 20 minutes before breakfast.” Specifying when, where, and how actions will occur increases follow-through rates significantly.
Environment design supports healthy choices. Keeping tempting foods out of the house, placing exercise clothes where they’re visible, and surrounding oneself with supportive individuals makes desired behaviors easier while reducing friction around unwanted habits.
Self-monitoring enhances awareness and accountability. Whether tracking food intake, physical activity, or blood glucose patterns, the act of recording behaviors increases mindfulness and reveals connections between actions and outcomes.
Anticipating obstacles and developing contingency plans prevents derailment. Identifying high-risk situations—holidays, vacations, stressful periods, social events—and creating specific strategies for navigating them maintains progress during challenging times.
Thriving Beyond Diagnosis: A New Normal 🌟
Many individuals discover that their Type 2 diabetes diagnosis, while initially devastating, ultimately catalyzes positive life changes extending beyond glycemic control. The discipline required for diabetes management often improves overall health, relationships, and life satisfaction.
Physical improvements frequently extend beyond blood sugar normalization. Weight loss, increased energy, better sleep quality, improved mood, and reduced joint pain commonly accompany effective diabetes management. Some individuals successfully achieve remission, maintaining normal blood glucose levels without diabetes medications, though continued lifestyle adherence remains essential.
The journey cultivates valuable skills applicable beyond health management: goal-setting, problem-solving, delayed gratification, resilience in the face of setbacks, and self-advocacy. These competencies enhance personal and professional life domains.
Developing expertise about nutrition, exercise physiology, and medical management often inspires individuals to help others facing similar challenges. Peer support, advocacy work, or even career changes toward health-related fields channel diabetes experiences into meaningful contributions.
Perspective shifts represent perhaps the most profound transformation. Rather than viewing diabetes as a limitation, many individuals reframe it as a catalyst for living more intentionally, prioritizing what truly matters, and appreciating each day. This mindset shift transforms burden into opportunity.
Continuing Education and Staying Informed 📖
Diabetes research advances rapidly, with new medications, technologies, and management strategies emerging regularly. Staying informed about developments enables individuals to optimize their management approaches and advocate for access to beneficial innovations.
Reputable information sources include professional organizations like the American Diabetes Association, medical journals, certified diabetes educators, and healthcare providers. Caution is warranted regarding unverified online sources, social media health claims, and miracle cure promises.
Participating in diabetes self-management education and support programs, whether upon diagnosis or years later, reinforces knowledge and introduces new concepts. These programs, often covered by insurance, provide structured learning and peer connection opportunities.
Clinical trials offer access to cutting-edge treatments while contributing to scientific knowledge. Individuals interested in participation can discuss options with healthcare providers or search registries like ClinicalTrials.gov for relevant studies.
The empowering journey through Type 2 diabetes ultimately transforms diagnosis from a frightening pronouncement into an opportunity for growth, improved health, and deeper self-understanding.
With resilience, knowledge, and proper support, individuals not only manage their condition effectively but often discover strengths and capabilities they never knew they possessed. The path forward, while requiring commitment and adaptation, leads toward a fulfilling life where diabetes occupies its proper place—managed, respected, but not defining.



